Good news for patients who don't respond to Cladribine. I found a study citation that shows that even for minor/non-responders to 2-CDA, complete remission after treatment with Rituximab was achieved.
A study at the University of Pisa, Pisa Italy, studied a cohort of 10 patients who followed a treatment regimen very similar to the one I'm in at NIH. Patients were first treated with a course of 2-CDA (chemo) followed by Rituximab 6 months later. Here's the study citation:
Purine analogues have dramatically improved the outcome of patients affected by hairy cell leukemia (HCL), although complete eradication of disease was achieved in few cases. The purpose of this study was to evaluate the role of Rituximab in eradicating minimal residual disease (MRD) in HCL patients after a pre-treatment with 2-chloro-deoxy-adenosine (2-CdA). Ten patients received four cycles of Rituximab after administration of Cladribrine. Before starting anti-CD20 antibody, two patients were in complete remission, six in partial remission and two showed no significant response to Cladribrine. All cases resulted IgH-positive. Median time from the last 2-CdA infusion was 5.7 months. Eight of 10 patients [four in partial remission (PR), two in complete remission (CR) and two unresponsive after 2-CdA] were evaluable for response. Two months after the end of anti-CD20 therapy, all evaluated patients presented a complete haematological remission. Moreover, Rituximab increased percentage of molecular remission up to 100% 1 yr after the end of treatment. Interestingly, in all cases but one, including those persistently polymerase chain reaction (PCR)-positive, semi-quantitative molecular analyses showed MRD levels lower than those found before Rituximab administration. Toxicity was very mild. The present results not only confirm the therapeutic effect of Rituximab, but also show its relevance in eradicating MRD in HCL.
The really great news here is that of 8 patients, 2 were non-responders at 6 months post-chemo, yet all achieved complete remission after treatment with Rituximab biological therapy, and the toxicity was very mild.
There is still plenty to hope for, and I'm glad I found the NIH study.
Friday, August 28, 2009
Wednesday, August 26, 2009
Plan B
A few months back I discussed how HCL thrives in the presence of a cytokine (cell signaling molecule) called tumor necrosis factor alpha (TNFa). Given my less than 3-sigma response to Cladribine, I thought it might be worth investigating foods and medicines that suppress the production of TNFa to help me bide my time.
I asked Dr. K (via e-mail) whether they monitor TNFa in the routine blood tests they perform. He said they used to but found the data to be not very meaningful. I assume this means there was too much variance in the data. I then asked him whether given the overall trend in my data, I'm considered a minor responder. He did not respond to that question.
I had read an article in Tallman and Poliak that discussed how TNFa reducing drugs given in parallel with 2-CdA improved response rates in HCL, so I did my own search regarding foods that lower TNFa and struck gold immediately.
As described in "Caffeine suppresses TNFa production via activation of the cyclic AMP/protein kinase A pathway", Horrigan et al, International Immunopharmacology, Vol. 4, No. 10-11 (October, 2004) pp. 1409-1417 -- coffee can suppress TNFa and thus may be helpful in suppressing the rate of cloning of HCL cells. The most caffeinated food (aside from sugar laden jolt and Red Bull) is restaurant prepared espresso. Here is the paper's abstract:
This study investigated the effect of in vitro exposure to caffeine, and its major metabolite paraxanthine, at concentrations relevant to typical caffeine consumption in humans, on lipopolysaccharide (LPS)-stimulated cytokine production in human whole blood. In addition, a role for the cyclic AMP/protein kinase A (PKA) pathway in the immunomodulatory effect of caffeine was investigated. Diluted whole blood (taken following >/=15 h abstinence from caffeine-containing food and beverages) was preincubated with caffeine or paraxanthine (10-100 microM) and stimulated with LPS (1 proportional, variant g/ml) for 24 h. The proinflammatory cytokines tumour necrosis factor (TNF)-alpha, interleukin (IL)-1beta and IL-12, and the antiinflammatory cytokine IL-10 were measured in cell-free supernatants. Whilst caffeine and paraxanthine had little or no effect on IL-10, IL-1beta, or IL-12 production, TNF-alpha production was suppressed in all individuals studied. The effect was statistically significant at 100 microM and consistent across seven experiments performed. Although not statistically significant, a similar effect was observed with paraxanthine. Caffeine (100 microM) also increased intracellular cyclic AMP concentrations in LPS-stimulated monocytes isolated from whole blood. Moreover, the effect of caffeine on TNF-alpha production was abolished by pretreatment with the protein kinase A inhibitor Rp-8-Br-cAMPS (10(-4) and 10(-5)M). To conclude, this study demonstrates that concentrations of caffeine that are relevant to human consumption consistently suppress production of the proinflammatory cytokine TNF-alpha in human blood and that this effect is mediated by the cyclic AMP/protein kinase A pathway.
I'm going to add one espresso a day to my morning routine in the hope that it will stop the strong cells from signaling further reproduction and infiltration of my marrow. With any luck, I might be able to tip the balance and hold off the stronger cells from reproducing while the chemo continues to take out the weaker ones. Then the Rituximab can come in and wipe out the cells that the chemo couldn't take out.
Foods containing Lutolein (a flavonoid) like celery, green pepper, and chamomile, also suppress TNFa. Other TNFa inhibitors include Nettle Leaf, and ECGC (found in Green Tea). Vitamin A also appears to help suppress TNFa production, which is also linked to the onset of diabetes ("Vitamin A may suppress type 1 diabetes", L. Crowley, Mar. 31, 2008).
I'll be adding all of these to my regular diet.
I wonder if previous studies of TNFa levels proved to be meaningless because diet can affect the levels. Without a controlled diet, studying TNFa levels may prove futile.
TNFa is also associated with demyelinating disorders such as multiple sclerosis and certain forms of tinnitus. Given the fact that Cladribine is effective in treating MS and HCL, I think a logical hypothesis is that Cladribine may somehow block TNFa signalling pathways, possibly by amplifying a protein kinase pathway. Perhaps in minor responders, there is a genetic difference which reduces this effect. A study of individuals who drank a V8-like beverage for 26 days showed they reduced their TNFa production by 34.4%.
Wish me luck!
I asked Dr. K (via e-mail) whether they monitor TNFa in the routine blood tests they perform. He said they used to but found the data to be not very meaningful. I assume this means there was too much variance in the data. I then asked him whether given the overall trend in my data, I'm considered a minor responder. He did not respond to that question.
I had read an article in Tallman and Poliak that discussed how TNFa reducing drugs given in parallel with 2-CdA improved response rates in HCL, so I did my own search regarding foods that lower TNFa and struck gold immediately.
As described in "Caffeine suppresses TNFa production via activation of the cyclic AMP/protein kinase A pathway", Horrigan et al, International Immunopharmacology, Vol. 4, No. 10-11 (October, 2004) pp. 1409-1417 -- coffee can suppress TNFa and thus may be helpful in suppressing the rate of cloning of HCL cells. The most caffeinated food (aside from sugar laden jolt and Red Bull) is restaurant prepared espresso. Here is the paper's abstract:
This study investigated the effect of in vitro exposure to caffeine, and its major metabolite paraxanthine, at concentrations relevant to typical caffeine consumption in humans, on lipopolysaccharide (LPS)-stimulated cytokine production in human whole blood. In addition, a role for the cyclic AMP/protein kinase A (PKA) pathway in the immunomodulatory effect of caffeine was investigated. Diluted whole blood (taken following >/=15 h abstinence from caffeine-containing food and beverages) was preincubated with caffeine or paraxanthine (10-100 microM) and stimulated with LPS (1 proportional, variant g/ml) for 24 h. The proinflammatory cytokines tumour necrosis factor (TNF)-alpha, interleukin (IL)-1beta and IL-12, and the antiinflammatory cytokine IL-10 were measured in cell-free supernatants. Whilst caffeine and paraxanthine had little or no effect on IL-10, IL-1beta, or IL-12 production, TNF-alpha production was suppressed in all individuals studied. The effect was statistically significant at 100 microM and consistent across seven experiments performed. Although not statistically significant, a similar effect was observed with paraxanthine. Caffeine (100 microM) also increased intracellular cyclic AMP concentrations in LPS-stimulated monocytes isolated from whole blood. Moreover, the effect of caffeine on TNF-alpha production was abolished by pretreatment with the protein kinase A inhibitor Rp-8-Br-cAMPS (10(-4) and 10(-5)M). To conclude, this study demonstrates that concentrations of caffeine that are relevant to human consumption consistently suppress production of the proinflammatory cytokine TNF-alpha in human blood and that this effect is mediated by the cyclic AMP/protein kinase A pathway.
I'm going to add one espresso a day to my morning routine in the hope that it will stop the strong cells from signaling further reproduction and infiltration of my marrow. With any luck, I might be able to tip the balance and hold off the stronger cells from reproducing while the chemo continues to take out the weaker ones. Then the Rituximab can come in and wipe out the cells that the chemo couldn't take out.
Foods containing Lutolein (a flavonoid) like celery, green pepper, and chamomile, also suppress TNFa. Other TNFa inhibitors include Nettle Leaf, and ECGC (found in Green Tea). Vitamin A also appears to help suppress TNFa production, which is also linked to the onset of diabetes ("Vitamin A may suppress type 1 diabetes", L. Crowley, Mar. 31, 2008).
I'll be adding all of these to my regular diet.
I wonder if previous studies of TNFa levels proved to be meaningless because diet can affect the levels. Without a controlled diet, studying TNFa levels may prove futile.
TNFa is also associated with demyelinating disorders such as multiple sclerosis and certain forms of tinnitus. Given the fact that Cladribine is effective in treating MS and HCL, I think a logical hypothesis is that Cladribine may somehow block TNFa signalling pathways, possibly by amplifying a protein kinase pathway. Perhaps in minor responders, there is a genetic difference which reduces this effect. A study of individuals who drank a V8-like beverage for 26 days showed they reduced their TNFa production by 34.4%.
Wish me luck!
Monday, August 24, 2009
Keep on Truckin'
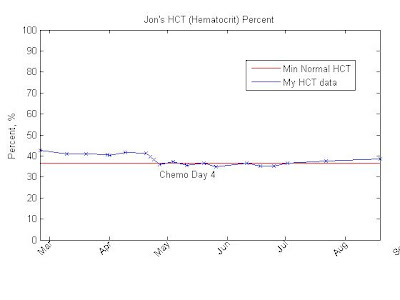
 I underwent chemotherapy (Cladribine -- aka Leustatin) four months ago and although 99% of the malignant cells in my peripheral blood have died off, my bone marrow response has been very slow. Dr. K wants me to remain on a one-month blood work follow up. As you can see in the graph below, my platelet count is still hovering around 100. I think that the count may be deceptively low because the platelets may be aggregating and fooling the FACS into counting what are multiple aggregate platelets as a single platelet. I'm going to ask Dr. K if he can order a peripheral smear slide examination (direct microscope examination by a pathologist) to see if this might be the case.
I underwent chemotherapy (Cladribine -- aka Leustatin) four months ago and although 99% of the malignant cells in my peripheral blood have died off, my bone marrow response has been very slow. Dr. K wants me to remain on a one-month blood work follow up. As you can see in the graph below, my platelet count is still hovering around 100. I think that the count may be deceptively low because the platelets may be aggregating and fooling the FACS into counting what are multiple aggregate platelets as a single platelet. I'm going to ask Dr. K if he can order a peripheral smear slide examination (direct microscope examination by a pathologist) to see if this might be the case.
 The good news is that my WBC, RBC, neutrophil and other counts continue to increase, although slowly. Some other counts, like Basophils, that were previously imperceivable, have now started registering.
The good news is that my WBC, RBC, neutrophil and other counts continue to increase, although slowly. Some other counts, like Basophils, that were previously imperceivable, have now started registering. Full disclosure -- I took 100 mg of grape seed extract (GSE) per day for a week back in June -- after my platelets had gone to 131, but before the next test showed them crashing back down to 100. Dr. K didn't have a problem with it (probably because he doesn't think it'll do anything), but given GSEs apoptotic effects on Jurkat leukemia cells, I thought it might also help destroy HCL cells too. The studies conducted by City of Hope indicated that GSE wouldn't harm healthy cells; however, I'm concerned that the GSE might have somehow knocked down my bone marrow's progenitor cell production. Still, there hasn't been enough data collected on GSE's effects in humans to know for sure.
I found an article addressing the efficacy of injecting Cladribine intravenously -- "Treatment of hairy cell leukemia with cladribine (2-Cda) by subcutaneous bolus injection: a phase II study," by Rohr et al, Annals of Oncology, 2002. I believe it is the basis for Dr. K's decision to use this method of administration in his clinical trial. The median time to failure for this approach is approximately 38 months. That sounds bad, but I think what it really means is that once a complete remission is achieved, it usually takes 38 months before any malignant cells are detected again. It may take much longer before the marrow and blood counts are affected, requiring a second round of chemotherapy.
Using this approach resulted in an overall remission rate of 97% (76% complete, 21% partial). Complete response requires the dissapearance of all evidence of disease, a return to normal peripheral blood counts, and the absence of hairy cells in the blood stream and the bone marrow. Time to failure is defined as the time between treatment start and progression, relapse, second tumor, or death, whichever occurs first. A partial response also requires a return of all blood counts to normal, but the reduction of cells in the marrow is somewhere between 50 and 99 percent.
PRs and CRs usually occur within 10 weeks after chemotherapy, so I'm bummed because it's been 16 weeks and my blood counts are still below normal and malignant cells, however slight, are still being detected in my bloodstream. That makes me part of the 5% considered minor/no response, so I'm glad I'm in the trial. Hopefully, what the Cladribine doesn't kill, the Rituxan I'm getting in October (once a week for 8 weeks) will.

(More at the bottom of this blog post...)




 I've lost a total of 16 pounds over the last two months -- mostly excess fat. I'm down to 188 pounds and holding steady now. My endurance is great, but I have been feeling dizzy lately. I'm anxious for my next bone marrow biopsy in October and to get started on the Rituxan.
I've lost a total of 16 pounds over the last two months -- mostly excess fat. I'm down to 188 pounds and holding steady now. My endurance is great, but I have been feeling dizzy lately. I'm anxious for my next bone marrow biopsy in October and to get started on the Rituxan.I also have a theory on what may have caused my leukemia. Several fellow HCLers have written to me noting that they are also RF engineers or hobbyists, wondering if there may be a common association between our line of work and the disease. A common factor in all of us is that we experienced high-power RF burns over 10 years ago. Likewise, electrical linemen also seem to have a slightly higher incidence of leukemia. Back in 1998, I received a 20 to 40 Watt RF burn at 137.5 MHz when a fellow engineer indicated he had turned off a transmitter but had not. When I disconnected the transmitter's output cable to reconfigure the system for another test, I received a severe RF burn on my hands that took several weeks to heal. In some people, RF burns may cause cellular mutations and induce HCL, but until some meaningful data is collected to prove this, I won't know for sure.
Regardless, bad things happen every day. You just have to accept it and keep on trucking.
KOT!
Tuesday, August 18, 2009
The Cost of Hairy Cell Leukemia
I reviewed all my insurance statements since my first doctor's appointment that led to my diagnosis and treatment for HCL. The total diagnostic cost billed by the doctors was $19250. Add the "virtual" cost of the NIH provided chemo at $5,000, the 1-month BMB at $1500 and the follow-on CBCs at $2000 along with $2500 for "progeny insurance" and the total is around $30260.
The insurance negotiated diagnostic costs came in at $4120 -- a $15,130 savings vice the doctor charges.
Given that I haven't submitted my "progeny insurance" claims yet, my total out-of-pocket (OOP) expense thus far is $2695. A savings of $42565, which may increase when I submit the other claims. My total OOP expense could be as low as $195. Not bad. Say what you want about insurance companies, but I'm grateful for mine. Without their negotiations and coverage, HCL would have left me bankrupt.
What I don't understand is why the initial doctors costs are so high compared to the negotiated costs. The variance between insured negotiated costs and uninsured non-negotiated costs is beyond reason. That the people who can afford it the least are left paying the most when their health turns for the worse is immoral given the large arbitrary cost fluctuations that exist between the insured and non-insured.
Following up on my last blog, my ALT and AST levels after going off Clonazepam were very good -- 24 and 28, respectively, so I've switched from Clonazepam to Gabapentin, which doesn't metabolize. I go in for my 4-month CBC tomorrow. I'll post the results once I get them.
The insurance negotiated diagnostic costs came in at $4120 -- a $15,130 savings vice the doctor charges.
Given that I haven't submitted my "progeny insurance" claims yet, my total out-of-pocket (OOP) expense thus far is $2695. A savings of $42565, which may increase when I submit the other claims. My total OOP expense could be as low as $195. Not bad. Say what you want about insurance companies, but I'm grateful for mine. Without their negotiations and coverage, HCL would have left me bankrupt.
What I don't understand is why the initial doctors costs are so high compared to the negotiated costs. The variance between insured negotiated costs and uninsured non-negotiated costs is beyond reason. That the people who can afford it the least are left paying the most when their health turns for the worse is immoral given the large arbitrary cost fluctuations that exist between the insured and non-insured.
Following up on my last blog, my ALT and AST levels after going off Clonazepam were very good -- 24 and 28, respectively, so I've switched from Clonazepam to Gabapentin, which doesn't metabolize. I go in for my 4-month CBC tomorrow. I'll post the results once I get them.
Subscribe to:
Posts (Atom)